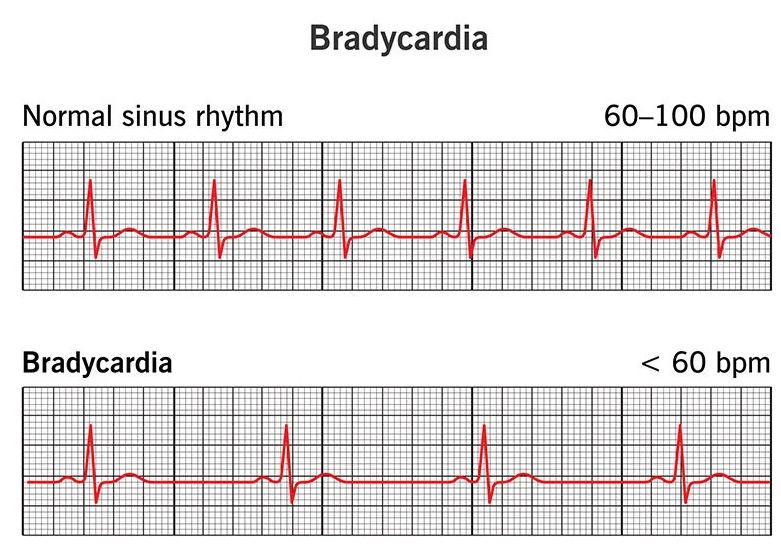
Bradikardija se definira kao očekivana frekvencija srčanih otkucaja manja od 60 u minuti. Može biti fiziološka (npr. kod sportaša), kardijalnog porijekla (atrioventrikularni blok ili bolest sinusa), nekardijalnog porijekla (vazovagalna reakcija, hipotermija, hipotireoza, hiperkalemija) ili uzrokovana lijekovima. Normalna brzina otkucaja srca kod odraslih kreće se između 60 i 100 otkucaja u minuti.
Pacijenta treba procijeniti koristeći pristup ABCDE. Bitno je identificirati uzroke bradikardije i utvrditi postoje li neželjeni znakovi. Ako su prisutni neželjeni znakovi, treba započeti liječenje bradikardije.
NEŽELJENI ZNAKOVI:
- Sistolički tlak
- Frekvencija srčanih otkucaja
- Ventrikularne aritmije koje narušavaju krvni tlak i zahtijevaju liječenje
- Oštećena srčana funkcija
AKO JE PRISUTAN JEDAN ILI VIŠE NEŽELJENIH ZNAKOVA:
- Uspostaviti venski pristup
- Primijeniti kisik
- Postaviti EKG monitor (kontinuirano praćenje)
- Izvršiti EKG s 12 derivacija
- Praćenje zasićenosti kisikom
- Praćenje i kontrola krvnog tlaka
- Pripremiti i primijeniti atropin (0,5 mg atropina IV, ako je potrebno, ponoviti svakih 3-5 minuta do maksimalno 3 mg)
- Transport do bolnice
- OPREZ! Ako postoji akutna ishemija miokarda ili akutni infarkt miokarda
Ako lijekovi ne djeluju, razmotrite neinvazivno kardiostimuliranje.
Kod bradikardije s neželjenim znakovima uzrokovanim infarktom miokarda dijafragme koji ne reagira na atropin, bradikardije zbog ozljeda kralježnice i primatelja presađenog srca, razmotrite primjenu aminofilina.
Za stabilne pacijente bez neželjenih znakova ili one koji dobro reagiraju na atropin, razmislite o riziku od asistole.
AKO POSTOJI RIZIK OD ASISTOLIJE:
- Nedavna asistolija
- Mobitz tip II AV blok
- Potpuni AV blok (treći stupanj), posebno s širokim QRS kompleksom ili učestalošću Ventrikularna aritmija >3 sekunde
- Pokrenite transkutano kardiostimuliranje ako nema odgovora na atropin, a pacijent ostaje nestabilan s znakovima cirkulacijskog zatajenja.
- Pratite pacijenta i pokušajte utvrditi uzrok bradikardije.
- Ako transkutano kardiostimuliranje nije odmah dostupno ili nije djelotvorno, razmotrite primjenu epinefrina.
Korištena literatura: Smjernice za predbolničku hitnu medicinsku službu, Smjernice ERC-a iz 2011. godine